Introduction to Tuberculosis
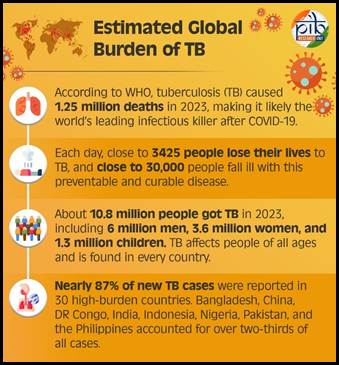
Tuberculosis, or TB, is an infectious disease that most often affects the lungs. It is caused by a bacterium called Mycobacterium tuberculosis. Though it can be treated and cured, TB continues to be one of the leading causes of death from infectious diseases worldwide. In India, the burden remains high despite decades of public health efforts.
TB is not just a health challenge. It impacts families, communities, and the country's economy. People from low-income backgrounds often face barriers in accessing timely diagnosis and treatment. Malnutrition, poor living conditions, and limited healthcare access create a cycle that makes prevention and recovery harder. In this sense, TB is both a medical concern and a social one.
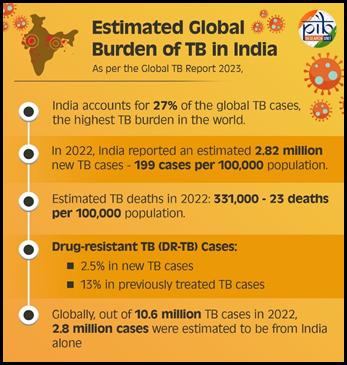
India accounts for a significant share of the world's TB cases. Tackling it requires more than medical treatment - it demands public awareness, community participation, and strong government action. Over the years, national programs have evolved to address TB control. Still, challenges like drug resistance, stigma, and underreporting persist.
We will understand what TB is, how it spreads, and how it affects both individuals and society. It also breaks down the symptoms to watch for, how the disease is diagnosed, and the treatment options available. In the later sections, we'll cover India's strategy to eliminate TB and the ongoing government initiatives working toward that goal. Together with government support, we can fight the disease to eradicate it.
What Is Tuberculosis (TB)?
Tuberculosis is a bacterial infection caused by Mycobacterium tuberculosis. It most commonly affects the lungs. This form is called pulmonary TB. However, the infection can also occur in other parts of the body, such as the brain, spine, lymph nodes, or kidneys. These are known as extrapulmonary forms of TB and may show different symptoms depending on the organ involved.
TB spreads through the air when a person with active TB in their lungs coughs, sneezes, speaks, or spits. Tiny droplets containing the bacteria can stay suspended in the air for hours. People nearby can breathe in these droplets and become infected. However, it is important to note that not everyone who breathes in the bacteria will fall ill.
The infection can exist in two forms: latent TB and active TB. In latent TB, the person carries the bacteria in their body, but it remains inactive. They do not show symptoms and cannot spread the disease. However, latent TB can become active later, especially if the person's immune system becomes weak.
In active TB, the bacteria multiply and cause symptoms such as a persistent cough, weight loss, fever, and night sweats. Only people with active pulmonary TB are contagious. This is why early diagnosis and proper treatment are essential not just for the patient's recovery but also for stopping the spread to others.
Understanding this difference between latent and active TB is crucial for effective control and prevention. Both forms need medical attention, though the approach differs. Identifying and treating latent TB can prevent future cases of active disease and reduce the overall burden in high-risk populations.
Types of Tuberculosis
Tuberculosis can affect different parts of the body and vary based on drug resistance. Here are the main types:
- Pulmonary TB: This is the most common form and affects the lungs. It is also the most infectious type, spreading through airborne droplets when a person with active TB coughs or sneezes. Symptoms include persistent cough, chest pain, and coughing up blood.
- Extrapulmonary TB: Occurs when TB spreads beyond the lungs. It can affect the brain, spine, kidneys, lymph nodes, or bones. Symptoms depend on the affected organ and may not always be easy to detect.
- Miliary TB: A rare but serious form, miliary TB happens when the bacteria enter the bloodstream and spread throughout the body. It can cause multiple organ failure and needs urgent treatment. The name comes from its millet-seed-like pattern seen on chest X-rays.
- Drug-sensitive TB: This form responds well to standard first-line TB medicines, such as isoniazid and rifampicin. Treatment usually lasts for six months and has a high success rate when followed properly.
- Multidrug-resistant TB (MDR-TB): Caused by bacteria that do not respond to at least isoniazid and rifampicin. Treating MDR-TB is more complex, requiring second-line drugs that may cause more side effects and require longer treatment periods.
- Extensively drug-resistant TB (XDR-TB): A more dangerous form of MDR-TB, XDR-TB is also resistant to key second-line drugs like fluoroquinolones and injectable agents. Treatment options are limited, expensive, and less effective.
- HIV-associated TB: People living with HIV are at much higher risk of developing TB due to weakened immunity. TB in these individuals may be harder to detect and treat, and often presents in less typical ways.
Who Is Affected by TB?
TB can affect anyone, but some groups face a higher risk due to health, living conditions, or lifestyle.
People with weak immune systems, such as those living with HIV, undergoing cancer treatment, or taking immunosuppressants, are more likely to develop active TB. Malnourished individuals, especially children and the elderly, are also vulnerable.
Overcrowded areas with poor ventilation increase exposure risk, making residents of slums and densely populated communities more susceptible. Healthcare workers are at risk due to regular contact with infected individuals.
Lifestyle factors like smoking, alcohol abuse, and unmanaged diabetes further weaken immunity and increase TB risk.
While TB affects both men and women, it is more commonly reported in men. However, women often face delays in diagnosis due to social or healthcare barriers.
Children and older adults require special attention, as TB can progress more quickly and severely in these age groups.

Symptoms of TB
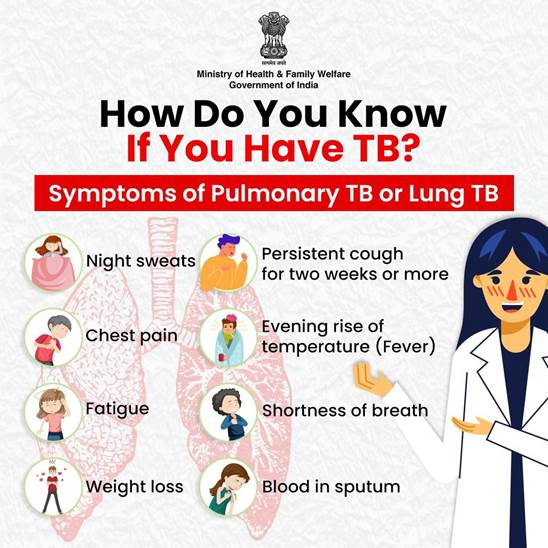
Pulmonary TB
- Chronic cough lasting more than two weeks
- Coughing up blood or sputum
- Pain in the chest while breathing or coughing
- Night sweats that soak clothes
- Constant fatigue or tiredness
- Noticeable weight loss without trying
- Fever that comes and goes
Extrapulmonary TB
Symptoms depend on the organ affected, such as:
- Persistent back pain in spinal TB
- Swollen and sometimes painful lymph nodes
- Seizures or headaches in TB meningitis
Diagnosis and Test for Tuberculosis
Diagnosing TB involves a mix of clinical tests and imaging.
- The sputum microscopy test is the most basic method to detect TB bacteria.
- CB-NAAT or GeneXpert is a rapid molecular test that confirms TB and checks for drug resistance.
- A chest X-ray helps detect lung involvement.
- Tuberculin Skin Test (Mantoux) and Interferon Gamma Release Assays (IGRAs) check for TB infection, especially in latent cases.
- CT or MRI scans are used for detecting extrapulmonary TB.
- In cases involving bones, lymph nodes, or other organs, biopsy or fluid aspiration may be needed.
Early and accurate diagnosis is critical for effective treatment and preventing further spread in the community.
Treatment and Remedies of Tuberculosis
Treatment for TB depends on the type of infection and drug resistance.
Drug-sensitive TB follows a 6-month regimen:
- Intensive phase (2 months): A combination of four medicines-isoniazid (H), rifampicin (R), pyrazinamide (Z), and ethambutol (E)
- Continuation phase (4 months): Only isoniazid and rifampicin (HR)
This is administered under the DOTS strategy (Directly Observed Treatment Short-course) within the National TB Elimination Programme (NTEP). Adherence to the full course is essential to prevent relapse or drug resistance.
Multidrug-resistant TB (MDR-TB) and Extensively drug-resistant TB (XDR-TB) require longer, more complex treatment, typically 18 to 24 months. Drugs include bedaquiline, linezolid, clofazimine, and delamanid, among others. These regimens have a higher risk of side effects, such as liver problems or hearing loss. WHO and NTEP provide detailed treatment guidelines for these cases.
TB-HIV co-infection needs special care. Antiretroviral therapy (ART) is started alongside TB treatment. The choice of medicines is carefully planned to avoid drug interactions and ensure both infections are managed effectively.
Timely diagnosis and adherence to treatment not only cures the patient but also helps stop further spread in the community.
Fatality and Long-Term Impact
TB remains one of the top ten causes of death worldwide. Drug-resistant forms like MDR-TB and XDR-TB carry higher risks of fatality, especially without early treatment. Delayed diagnosis can lead to complications, prolonged illness, and wider transmission. Even after recovery, many patients suffer long-term lung damage. In HIV-positive individuals, TB can be more aggressive and harder to treat. Stigma surrounding TB also causes people to delay seeking care, increasing the risk of severe illness and death.
Prevention and Control Measures
Preventing TB involves medical, environmental, and social efforts. The BCG vaccine, given to infants, offers protection against severe forms of TB in childhood.
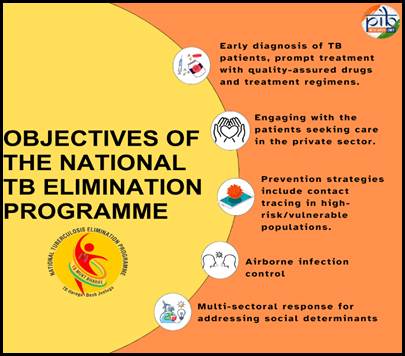
Early detection is key. Screening high-risk groups and ensuring timely diagnosis through sputum and molecular tests helps control the spread. TB Preventive Treatment (TPT) is recommended for those at high risk, such as household contacts of TB patients, people living with HIV, and those with other immune-compromising conditions.
Improving living conditions plays a major role: good nutrition, proper ventilation, and hygiene reduce risk. Cough etiquette and wearing masks in crowded places can limit airborne transmission.
Regular checkups for people with HIV or chronic illness help in early identification. Contact tracing and temporary isolation of infectious cases are also essential public health strategies.
Lastly, reducing stigma and misinformation is crucial. Open communication encourages early help-seeking, better compliance, and community support in TB control.
Government Schemes and Support for Tuberculosis in India
National TB Elimination Programme (NTEP)
A. Overview
The National TB Elimination Programme (NTEP)-formerly the Revised National TB Control Programme (RNTCP)-is now India's flagship national effort under the National Health Mission. Its goal: eliminate TB by 2025, five years ahead of global targets set in the WHO's End TB Strategy. The programme follows the pillars of the National Strategic Plan (2017–25): Detect, Treat, Prevent, and Build.
B. Key Interventions
- Free testing and quality-assured treatment are available to all patients across the country
- National implementation of DOTS and the recent shift to daily treatment regimens under NTEP
- Public–private partnerships, including provider interfaces and Nikshay Mitras, increase case detection and patient follow-up
- Active case-finding and contact tracing focus on vulnerable groups and high-risk areas
- Under Nikshay Poshan Yojana, patients now receive ₹1,000 per month (previously ₹500) via DBT for nutritional support
- Real-time monitoring via the Nikshay digital platform and App ensures patient tracking
C. Focus on Drug‑Resistant TB
- Special PMDT (Programmatic Management of Drug‑Resistant TB) units handle MDR‑TB and XDR‑TB
- Patients get access to newer TB drugs like bedaquiline, delamanid, linezolid, and clofazimine under expanded guidelines
- District-level labs now feature rapid molecular diagnostics, including CB‑NAAT (GeneXpert) and TruNAT, to detect resistance quickly
Government Schemes and Benefits for TB Patients
- Nikshay Poshan Yojana provides ₹1,000/month through Direct Benefit Transfer for the full duration of TB treatment
- Under Ayushman Bharat – PM‑JAY, eligible TB patients receive free hospitalization and treatment as needed
- Universal Drug Susceptibility Testing (UDST) is mandatory before starting TB therapy, helping detect resistance early
- Mobile diagnostic vans bring screening and CB‑NAAT services to remote and tribal areas
- All TB patients receive free drugs and diagnostics, whether treated at public centers or through private providers linked to NTEP
- TB Preventive Treatment (TPT) is offered to household contacts and other high-risk individuals
- The TB Champions programme educates and mobilizes communities, especially around stigma reduction
- Tailored support exists for patients with HIV-TB co‑infection, diabetes, and other comorbidities
Key Advances in Medical Science in India
India has made significant strides in scientific innovation and TB research:
- Genome sequencing: In March 2025, India announced completion of 10,000 genome sequences of Mycobacterium tuberculosis under the Dare2eraD TB initiative, enabling faster, precision treatments.
- Machine learning models: Researchers used national NIKSHAY data to develop predictive models with 98% recall and AUC‑ROC scores of 0.95, improving risk stratification and guiding patient care.
- Optical sensors & spectroscopy: Raman-spectroscopy-based tools combined with ML showed ~100% true-positive detection in trials, offering rapid, portable diagnostics.
- Truenat and handheld X‑rays: WHO‑endorsed Truenat point-of-care PCR systems and three indigenous handheld X‑ray devices by ICMR now support fast, low-cost screenings in remote areas.
These developments are reshaping TB diagnosis and treatment, especially in rural and resource-limited settings.
Major Steps in Gujarat, Bihar & Jharkhand
Gujarat
Gujarat has emerged as a leader in achieving TB targets:
- Under the 100‑Day Intensive TB Elimination Campaign launched in December 2024, over 4.42 lakh individuals were screened in 16 districts, leading to 95% of the NITI Aayog TB registration goal being met and a 91% treatment completion rate in 2024.
- Community mobilisation events with TB Champions, seminars, and cured-patient participation helped reduce stigma and encourage early help-seeking.
Bihar
Bihar has taken administrative and programmatic initiatives:
- The Governor urged Red Cross volunteers to adopt TB patients under the TB Mitra Yojana, emphasising nutritional and social support contributions worth ₹800 per patient.
- The state launched digital governance platforms (BPSMS) to streamline health services and support institutional TB efforts through e‑health tools.
Jharkhand
Jharkhand's progress includes:
- Declaration of 38 TB‑free panchayats, with Garhwa district leading, under NTEP's targeted interventions.
- Corporate and community collaboration: Usha Martin CSR efforts trained women health advocates and received state recognition for their TB outreach.
- Expansion of hygiene‑nutrition programs (FNHW) across 263 blocks, with self-help groups driving rural health change.
Major News Highlights and Awards for Tuberculosis
Recent News on TB in India
- India recently began rolling out the BPaLM regimen (bedaquiline + pretomanid + linezolid ± moxifloxacin) to treat drug‑resistant TB in just six months, showing fewer side effects and over 1,000 patients nationwide.
- This shorter regimen is considered safer and more effective than traditional 18–20‑month treatments, and is being offered under strict national guidelines.
- JJ Hospital in Mumbai and several public health centers are piloting BPaLM, with early reports of rapid improvement and minimal adverse effects.
International Collaboration & Support for TB Control in India
- The World Health Organization (WHO) continues to support India's NTEP strategies, including diagnostics, treatment protocols, and community engagement under the global End TB Strategy.
- The government collaborates with the Stop TB Partnership, USAID, and the Bill & Melinda Gates Foundation for technical and financial support toward surveillance and digital innovation in TB care.
- India also participates in networks like BRICS TB research platforms, enabling cross‑country data sharing and cooperative policy development to reduce TB transmission among migrants and mobile populations.
Rural Initiatives & Citizen Participation in TB Control
- ASHA workers are the backbone of rural TB screening, outreach, and stigma reduction under the 100‑Day Intensive Campaign, often visiting homes to mobilize screening among high‑risk groups.
- Operation ASHA, an NGO-supported initiative, delivers last‑mile TB treatment with tech-supported tracking like eCompliance and community-based care in villages and slums.
- Volunteers-Ni‑kshay Mitras, cured‑TB survivors, and community champions-play a key role in nutrition support, counselling, and helping patients stay on treatment.
Awards & Recognition for TB Elimination Efforts
- India received the WHO's appreciation for its leadership in TB elimination during the Stop TB Partnership Board meeting in 2023, where the country's innovation and scale-up in diagnostics and treatment were acknowledged.
- The Subnational Certification Scheme recognizes districts and states for achieving targets under the TB-free India campaign. Several districts like Niwari (Madhya Pradesh) and Budgam (Jammu & Kashmir) were certified TB-Free.
- Nikshay Mitras, volunteers who support TB patients, have been honored at various district-level and national events for their role in reducing stigma and dropout rates.
- ASHA workers were also recognized under the National TB Elimination Program for their frontline role in active case finding and follow-up care.
Past and Present Statistics on Tuberculosis in India
Tuberculosis remains one of India's deadliest infectious diseases. Even though it's curable, it continues to kill thousands each year. India has the highest TB burden globally and the COVID-19 pandemic made it worse.
A. Pre-2020: A Mixed Trajectory
India had made slow but steady progress in TB control before the pandemic:
- In 2015, India accounted for 23% of the world's TB cases.
- The National Strategic Plan (2017–25) aimed to eliminate TB by 2025, five years ahead of the global target.
- New TB cases (incidence) fell from 217 per 100,000 in 2015 to 193 per 100,000 in 2019.
- TB deaths also declined slowly, thanks to DOTS, free treatment, and better case detection.
B. 2020–2021: The COVID Disruption
When the pandemic hit, TB detection and care took a massive hit.
- In 2020, case notifications dropped by 25% due to lockdowns and overwhelmed health systems.
- India reported 1.8 million TB cases, down from 2.4 million in 2019, not because TB fell, but because it was underreported.
- TB deaths rose again due to delayed treatment and missed diagnoses.
- The India TB Report 2021 confirmed setbacks in testing, contact tracing, and follow-up.
C. 2022–2023: Catch-Up Phase
India pushed back hard with digital tracking (Ni-kshay), active case finding, and public-private coordination.
- In 2022, case notifications rebounded to 2.4 million, back to pre-COVID levels.
- The estimated incidence rate stood at 196 per 100,000 in 2022.
- TB-related deaths fell slightly due to faster diagnosis using CBNAAT and wider drug-resistance screening.
But gaps remain. Multidrug-resistant TB (MDR-TB) cases are still under control, but rising. Many patients still drop out during treatment due to side effects or social stigma.
D. Current Picture (2023–24)
The India TB Report 2024 highlights:
- 2.5 million cases were notified in 2023.
- Treatment success rate crossed 85% for drug-sensitive TB.
- Private sector reporting improved, nearly 37% of cases came from private hospitals.
- 108 districts were declared TB-free under the Ni-kshay Mitra and TB Mukt Bharat campaign.
Still, India accounts for about 27% of global TB cases; the highest share in the world.
E. Why TB Persists
Experts point to:
- Malnutrition and poor immunity in rural and urban poor populations
- Crowded housing and lack of ventilation in slums
- Delays in diagnosis, especially in private sector
- Rising drug-resistant TB cases due to incomplete treatment
- Social stigma causing people to hide illness
What Lies Ahead?
India's goal is to eliminate TB by 2025, but that looks unlikely without deeper reform in public health delivery. Better nutrition, universal access to free testing, and stigma-free awareness are essential — not just slogans.
What More Can Be Done
To eliminate TB by 2025, we need more than government programs-we need community action and system-wide change.
- Community-led education drives can help break myths, encourage early diagnosis, and reduce stigma. Local influencers and recovered patients can become TB ambassadors.
- School awareness programs should include TB education in health modules. Teaching children how to identify symptoms can lead to earlier help for family members.
- TPT (TB Preventive Treatment) must be scaled for all high-risk groups, especially household contacts, people with HIV, and undernourished populations.
- Better integration with HIV and diabetes care is essential. TB often co-exists with these diseases, and joint management can prevent severe complications.
- Rural and tribal districts need more doctors, mobile health vans, labs, and trained frontline workers. Most delays in diagnosis and treatment start here.
- All private hospitals and clinics must report TB cases. Making notification mandatory will reduce underreporting and improve monitoring through Nikshay.
- Continued funding from central and state governments, international donors, and public-private partnerships is crucial to sustain this momentum.
With these added efforts, the goal of a TB-free India of our Government will be successful.
Conclusion
TB remains one of India's toughest health battles. It's curable, but only when diagnosed early and treated completely. The government has stepped up with strong policies, digital tracking, and support schemes. Yet stigma, delayed care, drug resistance, and rural health gaps still hold us back. What's needed now is a full-society approach, where communities, health workers, and private clinics all take shared responsibility. With continued focus, funding, and public awareness, India can reach its goal of eliminating TB by 2025. But the clock is ticking. Ignoring the problem is no longer an option.
References
- World Health Organization (WHO) – Tuberculosis
https://www.who.int/news-room/fact-sheets/detail/tuberculosis - India TB Report 2024 – Ministry of Health and Family Welfare
https://tbcindia.gov.in - Official NTEP Portal (formerly RNTCP)
https://tbcindia.gov.in/index1.php?lang=1&level=1&sublinkid=4573&lid=3179 - Nikshay Dashboard and App
https://nikshay.in - NTEP Annual Report 2024
https://tbcindia.gov.in/showfile.php?lid=3682 - Standard TB Regimens – WHO Treatment Guidelines for DS-TB and DR-TB
https://www.who.int/publications/i/item/9789241550000 - NTEP Technical Guidelines for TB Treatment in India
https://tbcindia.gov.in/showfile.php?lid=3316 - Drug-resistant TB Management – WHO and NTEP
https://www.who.int/publications/i/item/9789240063198 - National AIDS Control Organization (NACO) – TB-HIV Collaborative Activities
http://naco.gov.in/tb-hiv-collaborative-activities - Nikshay Poshan Yojana – MoHFW
https://tbcindia.gov.in/showfile.php?lid=3317 - PM-JAY (Ayushman Bharat)
https://pmjay.gov.in - Programmatic Management of Drug-Resistant TB (PMDT)
https://tbcindia.gov.in/showfile.php?lid=3305 - TB Champions & Community Engagement
https://tbcindia.gov.in/showfile.php?lid=3654 - India: Record Drop in TB Cases (The Hindu)
https://www.thehindu.com/news/national/indias-tb-burden-drops/article67884958.ece - TB Case Finding Through AI – Times of India
https://timesofindia.indiatimes.com/city/bengaluru/ai-helps-detect-tb-in-rural-areas/articleshow/101205721.cms - USAID – TB Support in India
https://www.usaid.gov/india/global-health/tuberculosis